
The School Nurse Experiment
Across the country, plans for reopening schools this fall remain tentative and rife with problems.
How to safely bring students back into the classroom during the coronavirus pandemic is an open question. From a nursing history perspective, though, one solution is patently obvious: put a nurse in every school.
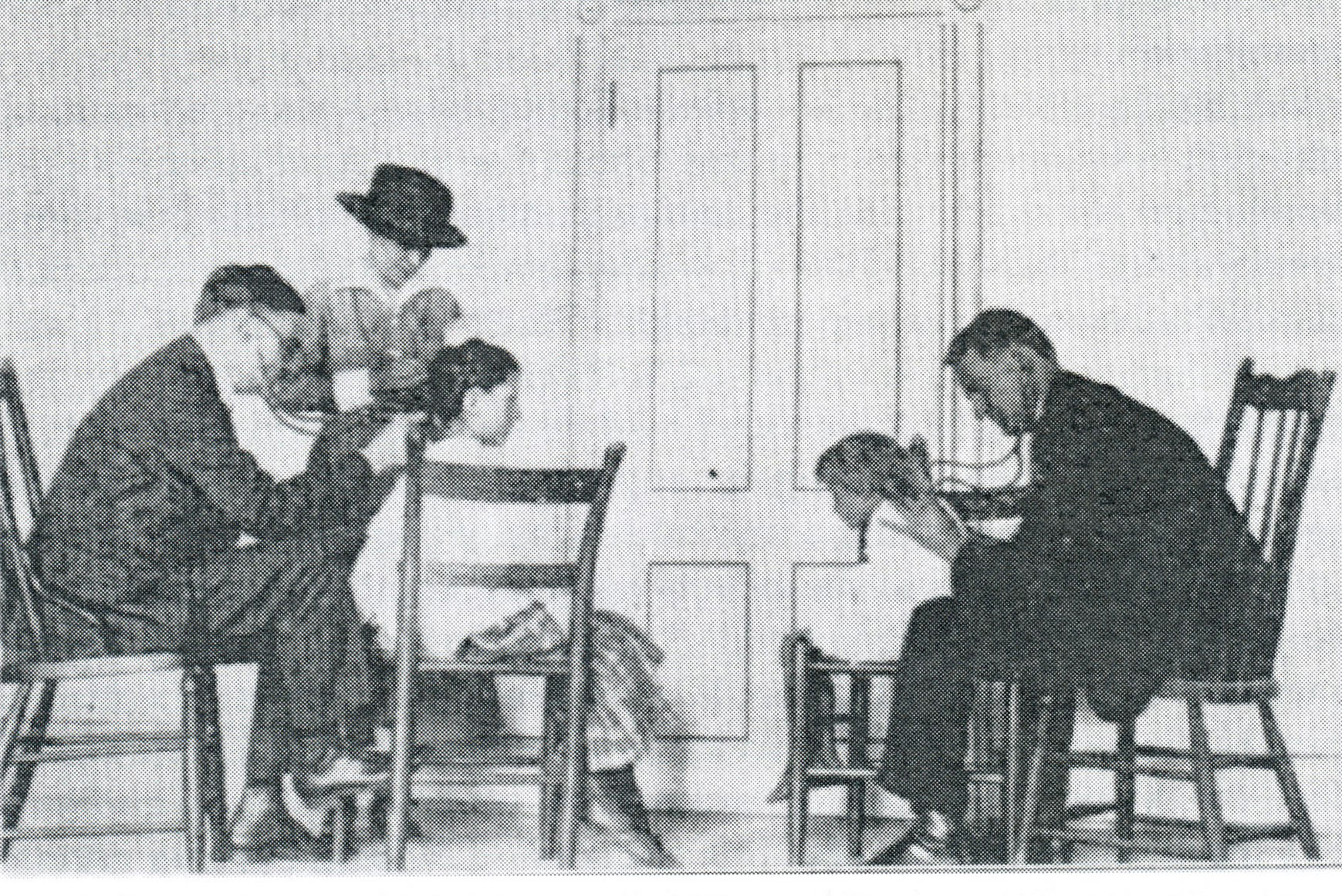

The school nurse gained entree into communities through her home visits, reaching isolated families to introduce them to the gospel of health and sanitation.
Bjoring Center for Nursing Historical Inquiry
A hundred years ago, school nurses taught children to wash their hands and use a handkerchief—and much, much more. They screened them for contagious diseases, quarantined those found to be infectious, and got the seriously ill to the doctor. They checked on sick children in their homes and taught parents how to care for them.
The school nurse also gained unique entree into communities through her home visits, reaching isolated families to introduce them to the gospel of health and sanitation. “In a great many cases, the children are the only means of reaching the homes, sometimes situated in such out of the way places that it is hard to find them,” said one school nurse in 1917.
And she was accorded the kind of welcome that was all but impossible for a health inspector knocking at the door. As one public health official in Virginia noted, “A nurse with this experience can go into the home without being regarded as an intruder and can do work utterly beyond the reach of the medical inspector.”
But budget cuts over the years have greatly reduced the ranks. Today, just 39.4% of U.S. schools employ a full-time school nurse. In 25% of those schools without a nurse, the care of sick or hurt children falls to an administrative assistant.
School nursing began as an experiment in 1902. Lillian Wald, founder of New York’s Henry Street Settlement, understood the challenges surrounding the lack of heath care for school children and its significance to the overall health of the community. Nurses had a huge potential role. Within a year, the number of children excluded from New York City schools for health reasons decreased by 90%; the school nurse was here to stay.
In Virginia, the school nursing experiment began in 1909 in Richmond, led by the Instructive Visiting Nurses Association. Working in two Richmond schools, nurse Ann Gulley examined 750 pupils and referred 291 of them to specialists. Under Gulley’s competent care, the attendance and health of students improved and the concept soon spread to other parts of Virginia. In Loudon County in northern Virginia, a group of concerned citizens in the Quaker church sponsored a school nurse experiment. Later, the county school board shared the cost of the nurse. Almost always, school health programs relied on a combination of private and public funding, stitched together from local boards of education, civic and religious organizations, parent-teacher associations, the local Red Cross, and philanthropic individuals.
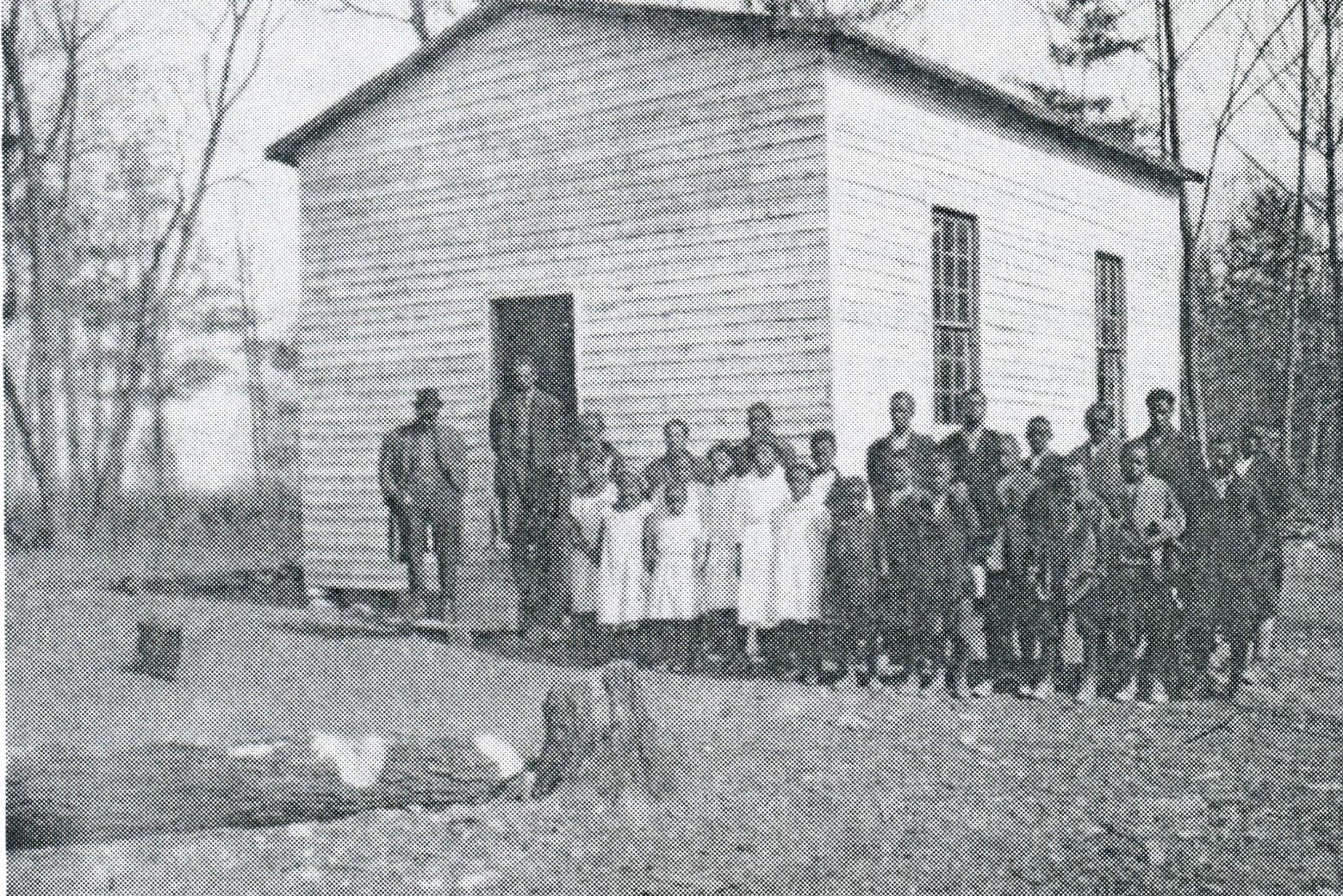
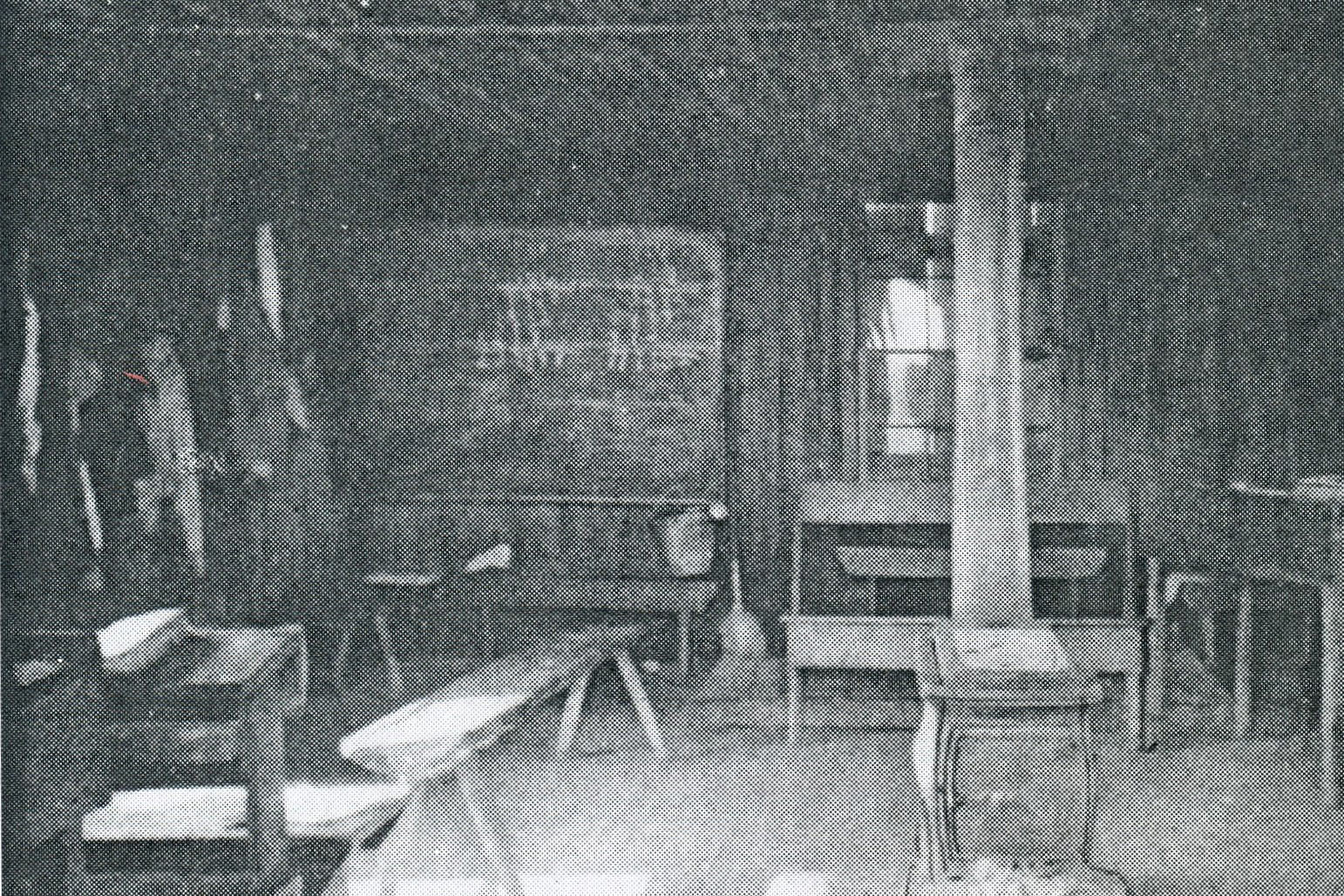
In the early twentieth century, children in rural schools had it worse than their urban counterparts. They often lacked clean drinking water and proper sanitation, and had little or no access to medical or nursing care. In many southern states, hookworm, pellagra, and malaria were endemic. Uncorrected conditions such as skeletal deformities, infected tonsils, and vision defects hindered their ability to learn. The one-room schools themselves were a serious problem, often without proper heat or ventilation.
A school nurse in Pittsylvania County, Va., reported on her work to help eradicate hookworm in 1920: “Loaded with two suitcases and portable scales, we drive up to a school house. The building is unpainted and rather dilapidated looking… After making a mental survey of pupils, we can usually give a good guess as to the infections to be found…should an infection be found, a notice is sent to the parents…If the treatment is indicated, we send it to him free, following the family up, examining, probably treating and curing them. Occasionally, we find children whose parents cannot read or write. These families we follow and endeavor to explain to them the importance of examination for hookworm.”
Vast distances and rough terrain added to the challenges facing the school nurse in rural areas. Some rode on horseback to reach their destinations. Followup duties included transporting children to medical clinics and hospitals. In 1923, Lillian Gorton, a nurse in Caroline County, Va., made a 170-mile round trip to Richmond with several charges. She transported a little girl with crossed eyes, an 11-year-old boy who was nearly blind, a child requiring a checkup for his eyes after receiving glasses, and a mother and her infant who needed surgery for a cleft palate. After delivering the mother and baby to the hospital, she accompanied the other children to their various appointments. During the trip, the car broke a spring, began leaking from the radiator, and blew out two tires. Having begun her day at 7 a.m., Gorton finally completed the trip at 10:30 in the evening, when she returned the last child home. All in a day’s work.
---
Sources: “School Nursing in Virginia: Hookworm, Tooth Decay, and Tonsillectomies,” by Mary E. Gibson, in Nursing Rural America: Perspectives From the Early 20th Century (Springer: 2015); and “The Importance of School Nurses in the Year of the Pandemic,” by Arlene Keeling, American Association for the History of Nursing, July 2020 President’s Message.
