Fear
in the spring, we were scared.
Fear
We knew very little about this virus. We didn’t know if we would run out of PPE, or if the PPE that we had was even effective. We were trained to carefully don and doff PPE to make sure we didn’t expose ourselves. If I slipped up on one step, I feared that I would catch this virus, which could potentially kill me, Lucas, or my coworkers, who were the only people I allowed myself to see for months. These fears kept me awake at night.
We knew very little about how to treat the virus, and we did things that hurt our patients when we were trying to help them. If we knew then what we know now, I would have put a lot fewer bodies into bags, and held up iPads for family members to see their loved ones in their last moments less often. I watched so many people, both younger than me, elderly, and all ages in-between die alone in ICU rooms with only a nurse in a space suit holding their hands while also titrating medications to keep them comfortable.
We knew very little about how to transform our Neuro and Cardiac ICU's into COVID ICUs overnight to accommodate daily surges in COVID-19 patients. I stayed up all night the night before my first night shift as a charge nurse of the CICU turned COVID ICU studying ARDS protocols and reading primitive COVID research articles. I knew how to keep a patient in cardiogenic shock alive, and how to troubleshoot balloon pumps, impellas, and LVADs, but I had little expertise in taking care of ARDS patients and how to prone them. We were scared and we knew very little, but we rose to the occasion. We picked up overtime, and spent our days off either restlessly sleeping or crying. Thankfully our communities listened, worked hard, and sacrificed so much to rise to the occasion alongside us to flatten the curve.
That was in the spring. We were all afraid, and we all knew very little but we got through it together.
Exhaustion
The summer was absolutely exhausting. Burned out nurses left our ICUs by the dozens, suffering from PTSD and an underwhelming response to the pandemic by systems that are meant to protect and support us. Once, while doing a huddle for the oncoming shift, I burst into tears in front of my coworkers because they were staffed so horribly for the night. It was the charge nurse's first shift off of orientation, and she was running with a full assignment, and the rest of the patients were staffed out of a safe ratio. There were also no CNAs.
Those in the community couldn’t understand why we were so tired, because for the most part COVID cases were manageable. Our hospital systems were failing us by not doing everything they could to get more nursing resources to us, while also asking us to do more and calling us "healthcare heroes" to try to make it all okay, and we were all still traumatized by the spring knowing full well what was to come.
Anger
Now, it is the fall. Hospital administrators were slow to listen to staffing concerns in the summer, but thankfully my hospital finally listened and invested in getting more hands on deck. But it is too little, too late. Nobody listened to us during the summer, and nobody is listening now. COVID is surging to new heights daily across the country, and we are being asked to do the same things now that we had to do in the spring. My unit is 100% COVID again. We are not consumed by fear like we were in the spring because we know so much more than we did then. Death rates are down because we have adapted protocols to treat COVID-19 patients, and we know that our PPE is mostly effective. This time, we are just angry, and by the way, people are still dying from this virus and the ripple effects it has had on our healthcare system. We are continuing to rise to the occasion despite being battered by nine months of trauma, but our communities are not rising to the occasion with us this time around. There is a false sense of security because death rates are down, and our community is not taking this seriously.
We are finite. We cannot continue to support these kinds of numbers of very sick patients. We are converting a third ICU to take care of COVID-19 patients at my hospital. All of our ICUs were typically filled to capacity pre-COVID. Even if someone doesn’t die from COVID right now, there is a high likelihood that they are dying from lack of access to a staffed ICU bed. We are cancelling and delaying elective procedures because we do not have the physical space to recover the patients. This is the healthcare system of a country that typically has the most resources out of any country in the world.
Nurses are usually characterized by being compassionate, caring individuals. In the last 24 hours, every nurse that I have talked to has told me that they wake up, and they are exhausted and angry. They come to work, and they are exhausted and angry. They go home, and they are exhausted and angry. This is such an uncomfortable feeling for me personally, as my response to hard situations has never been anger.
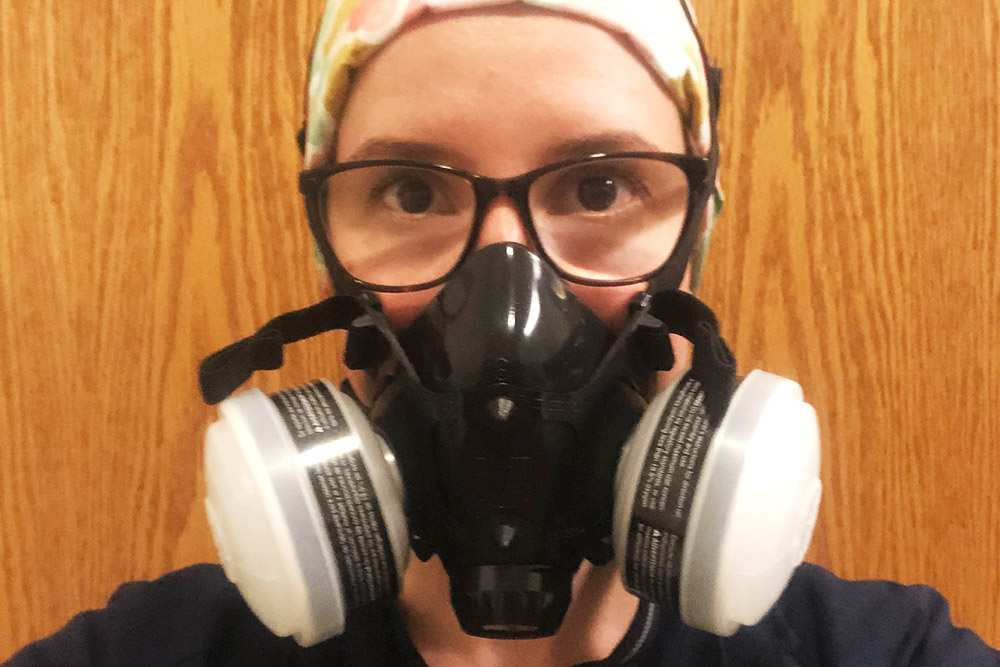
We were once afraid, but we are now traumatized, tired and angry. Our communities are failing us, because they are not sacrificing indoor events and social gatherings, and they are not wearing masks because they are uncomfortable. (As a side note: I encourage all those who think a cloth mask is uncomfortable to try wearing a half mask respirator for hours like we do).
I am begging you to stop, and listen to healthcare workers. We are not okay, this virus is not under control, and people are dying. Wear a mask, socially distance, and avoid indoor activities unless they are absolutely necessary. Before traveling for the holidays and seeing people from outside your immediate household, or not wearing a mask, consider how you are contributing to the spread of this virus, and how very selfish you are.

This essay, written by Denver, CO, nurse manager Kimmi Alderfer (BSN `14), was originally published on Alderfer's Facebook page on November 14, 2020. To date, it's been shared more than 300 times. Alderfer, who continues to work with COVID patients, says the pandemic has made her "less afraid to speak my true mind."
