
From the Archives
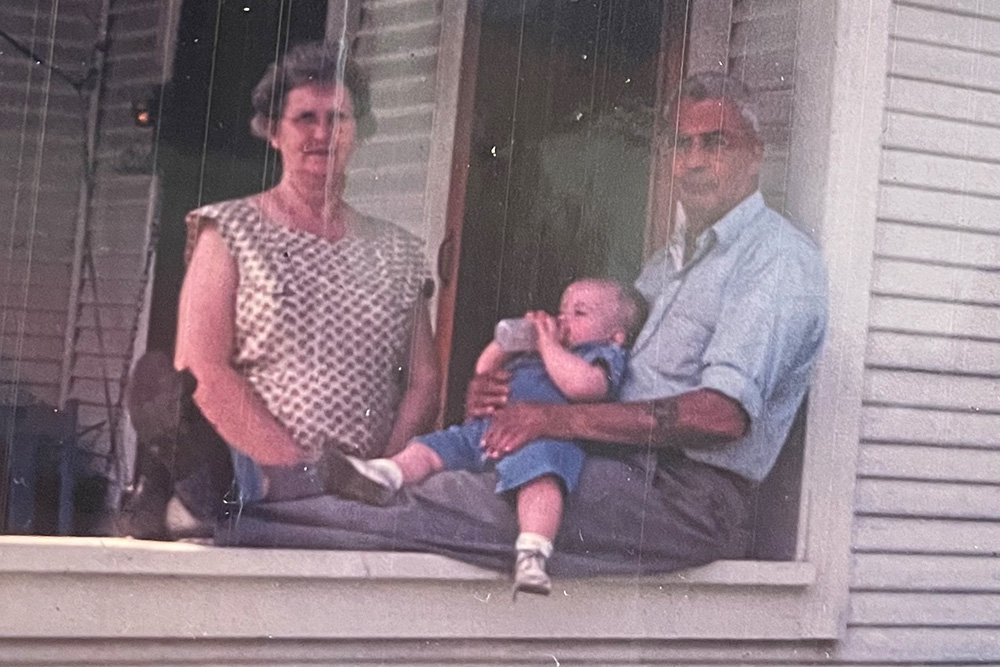
Kenneth R. White’s clinical experience began earlier than most—before, in fact, he even learned to drive.
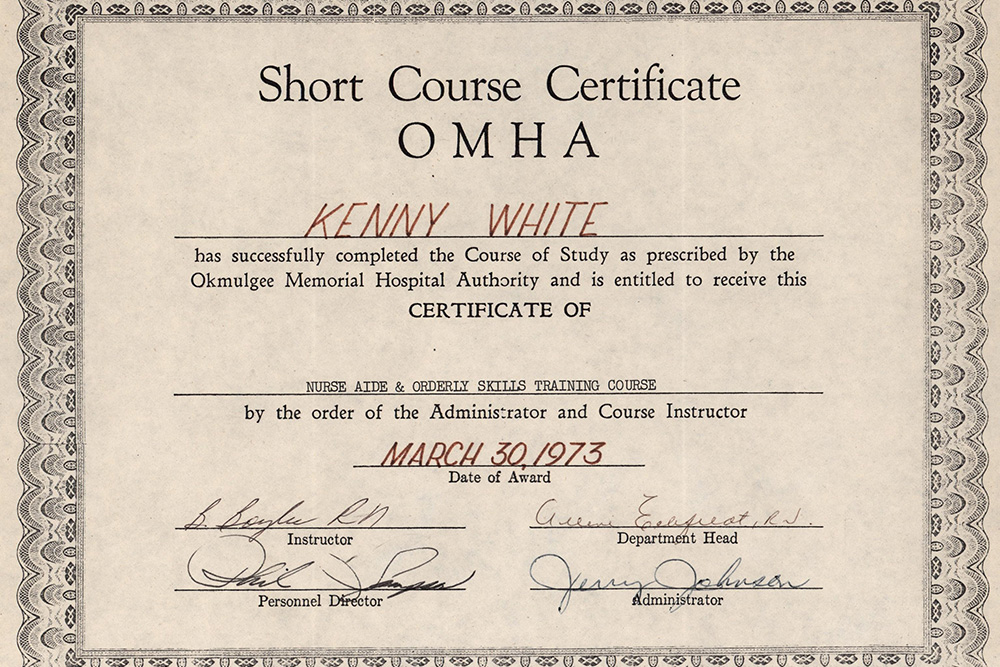
At age 16, White was already working full-time as an orderly at Okmulgee Memorial Hospital, in Okmulgee, OK, his hometown. There he ditched his book bag for the 3 p.m. to 11 p.m. shift and the princely wage of $1.73 an hour. It was 1972.
The time he spent at this rural Oklahoma hospital was more than an after-school job. It shaped his outlook and, rather quickly, set him on a path as a caregiver. In a recent oral history conducted with Bjoring Center director Dominique Tobbell, White (CERTI-AGACNP ’13) recalled seeing a patient suffer a horrendous death, his wishes ignored by medical staff, without family or anyone at his side to advocate for him.
“I just couldn’t get it out of my mind,” White said. “This is going to be my purpose. I need to be a voice for those people who don’t have a voice. That’s when I knew I wanted to be a nurse, or I wanted to do something to help vulnerable populations. I didn’t call it that then; I wasn’t that sophisticated.”




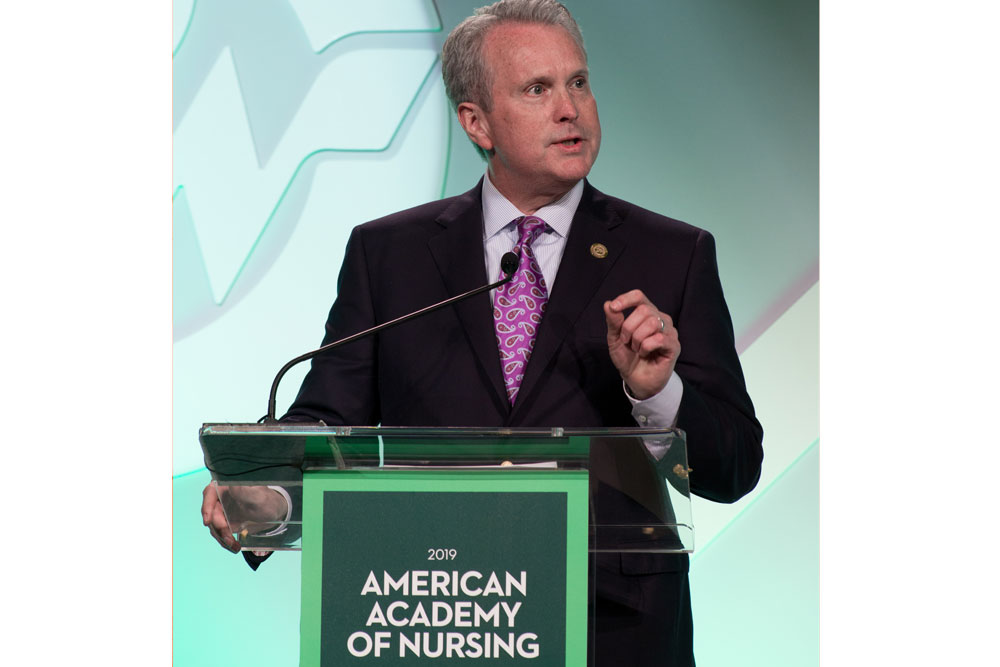
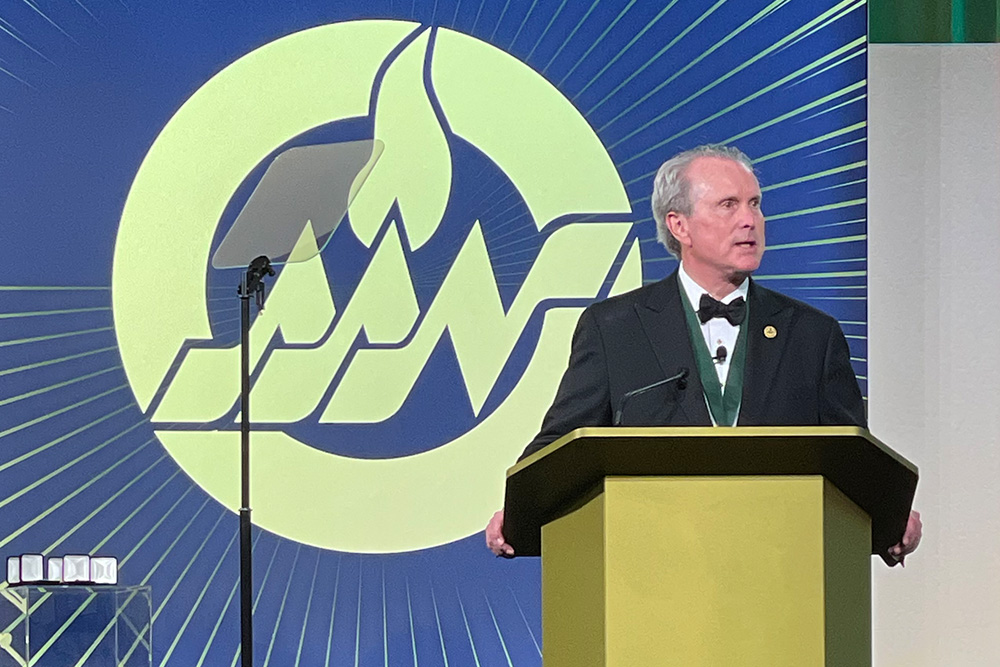
In 2021, White became the first man to serve as president of the American Academy of Nursing. A palliative care nurse practitioner and LGBTQ+ advocate, he is also dean of the Massachusetts General Hospital Institute of Health Professions School of Nursing. His papers are archived at the Bjoring Center for Nursing Historical Inquiry.
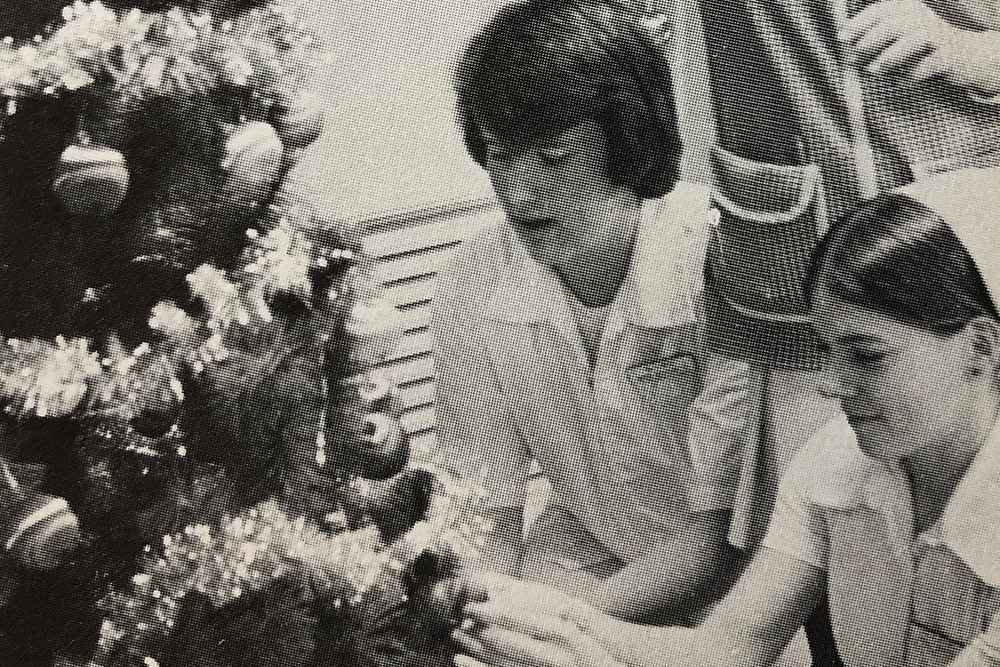
White had a multi-faceted career in healthcare administration before entering an accelerated nursing program in 1994, where he confronted old stereotypes that hadn’t died. The notion that “nursing is women’s work, and men just don’t get it” persisted, he said. A professor in one of his classes at Virginia Commonwealth University told students that, “’Nursing is a woman’s way of knowing.’ And I asked the question, ‘Well, where does that leave me? I want to know, too,’” White recalled.
Nursing is far from being gender balanced, though improvements have come with time. Male nurses today comprise about 12% of the national nursing workforce, compared to 2.2% in 1960, according to the U.S. Bureau of Labor Statistics. Most of that increase occurred in the last decade.
Soon after earning a BSN, White helped establish a walk-in clinic in 1999 at a church in downtown Richmond, Va., in partnership with Cross-Over Health Center. Every Friday, Centenary United Methodist Church provided free medical care to underserved community members, a number of whom were homeless and HIV-positive. It was staffed by two volunteers: White and physician Dr. Dianne Cane.
“I became very familiar with the homeless population, and they protected me,” he said. “They would see me on the streets. I loved them. And in my trunk, I kept a supply of shoes and coats and blankets and got all my friends to donate things. And I collected all these toiletries from the hotels. I still do this. And would hand them out to people at the clinic.”
White became certified as a palliative care nurse practitioner in 2013. That same year, he joined UVA’s School of Nursing as an associate dean for strategic partnerships and innovation, but he continued to carve out time for his practice, advocating at the bedside.

No tags found!
