
Giving Voice
The dream goes something like this:
Sydney Quigley (CNL `16) sees the little “c” by her name on the schedule. With a set of grey hospital scrubs from linen supply, she dresses and heads to the oncology floor to see her first patient—ventilated, sedated, pale—in bed, monitors humming a steady beat.
She looks closer. It’s her brother. Her stomach drops. Then she wakes up.
“We’re in a dark space all the time,” said Quigley, who works in acute/progressive care on an oncology floor in Richmond, and is often assigned to COVID patients. “Ten, 12 months ago, you had time to think about what you’d lost, the trauma, your experiences, one after the other. But now there’s no time to process, no relief. It’s just so heavy."
"You have to be done with something to be able to process. I’m still in survival mode; I just keep going.”
Becca Hedges Noonan, CNL `16, a COVID nurse manager in Richmond, Va.
As the pandemic grinds on, the virus mutates, and pockets of the country pulse with case spikes and troughs, nurses' traumas evolve, too. Those who’ve cared for COVID patients since the pandemic began are exhausted by vigilance. Staffing shortages and the all-hands-on-deck needs at many health systems can make nurses floated onto COVID units feel exploited and underappreciated. Many signed up with nurse staffing agencies, an increasingly lucrative alternative, and parachute into hotspots like soldiers in war. Others have seen their hours cut, and been forced to take side jobs to bolster diminished income. Many new nurses are shocked to find themselves experts at post-mortem care.
“I think it’s going to take years to unpack, but I’m just not in a place where I’m allowed to process yet,” said Becca Hedges Noonan (CNL `16), a COVID-unit nurse manager in Richmond. “You have to be done with something to be able to process. I’m still in survival mode; I just keep going.”
Heroes? Or Expendable?
What’s clear is that even with a new year, new vaccines, and new hope, nurses are overwhelmed and emotionally and physically exhausted. While some have sought support for their mental health, for many, the stigma of seeking such help persists. They’re tired of all the death. They’re tired of being tired. And in some cases, they’re tired of being nurses.
One-fifth of cardiac ICU charge nurse Kimmi Alderfer’s (BSN `14) nurse colleagues quit after Colorado’s first COVID spike last spring, a “bleed” that’s only been partially remedied by steep raises and hazard pay. Money isn’t a cure-all.
“You don’t eat, you don’t pee, you don’t sit down, you’re running constantly,” said Alderfer, who works in Denver, “and at the end of the day, you feel like you provided sub-optimal care. That sits with me. We don’t deserve that. Patients and families don’t deserve that. It keeps me awake at night to think about how tight it is right now, and where we are—and where we’re headed.”
“The tremendous turnover we’re seeing is heartbreaking,” said Jane Muir (BSN `16), a Charlottesville emergency room nurse, PhD student, and co-author of a recent essay titled “Are we heroes? Or expendable?” published in Ms. Magazine. “The people leaving are the ones who taught me to be a nurse. How are the new nurses going to learn if they’re not here?”
+60%
Increase, since 2018, in the number of U.S. travel nurses who are increasingly tapped to help with healthcare staffing
Given nursing’s historic recognition of burnout and moral injury, attrition has always been a concern, but COVID’s made the strain more palpable. With departures, a new generation of young nurses who’d believed they had more time to solidify their practice feel overwhelmed taking on new managerial roles and being considered the “senior” clinician. Many work required extra shifts, and pivot to constantly evolving roles. Health systems are increasingly turning to travel nurses to fill staffing gaps, which can create pressure and friction, given the significant differences in how they’re compensated.
“Many nurses feel betrayed,” said Dean Pamela Cipriano, “by an invisible enemy that has claimed patients’ lives and the lives of their colleagues, by a public that sometimes refuses to wear masks, or adhere to public health safety measures, and, early on, by the entire nation and its health systems for not providing adequate protection to keep them from getting infected while they selflessly cared for COVID patients.”
Constant waves of change bring fatigue, anger, and something else, too. More and more nurses have found their voices, individually and collectively, in a moment when the world appears ready to listen.
“Nurses aren’t always thought of as a particularly outspoken group, but the brutality of the pandemic has emboldened many to speak up,” said Cipriano. “We’re getting louder, and demanding change. We’ve become more insistent: don’t call us heroes for doing our jobs. Respect and listen to us. Include us in decision-making for solutions to address the ever-changing care challenges. Show us we’re valued for our expertise and commitment by taking care of us, and not just demanding we show up as conscripted workers.”
Like many of her peers, Alderfer spoke out on social media just before Thanksgiving, raging against the reckless gatherings she observed. That prompted apologies from friends and family, and recognition from caregiver peers. To date, her essay has been shared more than 300 times.
The pandemic “made me less afraid to speak my true mind,” said Alderfer. “I knew I was making other people uncomfortable with my anger but . . . it was also therapeutic. I wasn’t alone in what I was feeling. My coworkers told me they were wrestling with the same emotions.”
“Systems resilience doesn’t always help institutions make the margins they’re expected to meet,” said Tim Cunningham (CNL `09), vice president of practice and innovation at Emory Healthcare who wrote The Burden of Resilience Should Not Fall Solely On Nurses for the American Journal of Nursing. “But it’s not as hard as it sounds. Plus, should margins even be the goal if healthcare is really about healing people?"
Resilience can begin with simple practices, like what Cunningham calls the “neighborhood method.” Leaders ask people how they are, how their teams are, what specifically they need to do their jobs well—and then, within reason, deliver. In what is a turning moment for the profession, said Cunningham, people need to be heard, and not blamed if they’re hurting—a point others echoed.
"Yes, we have a business to run," said Scott Darrah (MSN `15), who's been on UVA Health's COVID-19 frontlines for nearly a year, and these days on-boards new nurses beginning in the Special Pathogens Unit, "but we have people to grow, too."
“It’s unrealistic for nurses and other clinicians to shoulder the responsibility to be resilient alone,” added Cipriano. “It’s up to health systems to create meaningful change and ensure a meaningful, supportive and empowering environment so we can be resilient.”
What’s In Their Toolbox
Through the pandemic’s turbulence, positive change and practice, like points of light, occasionally shimmer. Surveyed nurses recently reaffirmed interest in using gratitude, nature, and mindfulness to soothe stress, sentiments that align the Compassionate Care Initiative’s programming, which saw participation in its drop-in classes leap by 175% last spring, and 18% this fall and winter. Alongside popular “Compassion in Action” dialogues, yoga, meditation, virtual and in-person retreats, and visits with Kenny the therapy dog were other programs that aimed not to offer single experiences but to more fundamentally shift on-unit practices, attitudes, and behaviors, and bring resilience from the outside in.

Roving unit to unit, both in person and virtually, the Woodard Clinical Scholar Professor Richard Westphal (PhD `04) and Peggy Plews-Ogan of the Wisdom and Wellbeing team and eight Compassionate Care Initiative ambassadors fanned out across UVA Health to listen, connect, affirm, teach, and analyze. Against the pandemic’s early fears and more recent exhaustion, they taught concrete ways to tame stress, build professional and personal stamina, and manage loss and grief. Westphal schooled hundreds in stress continuum theory and the Stress First Aid approach, which helps people identify, approach, and connect troubled colleagues with resources and trains small groups of often-turned-to “peer support champions” to keep conversations and connectedness going through regular events.
“COVID has really stripped away the illusion that team members can keep sucking it up, and going back to work,” said Westphal. “That has never worked. This is about changing the culture.”
The Wisdom and Wellbeing team deployed a resource-rich web site, framed a system-wide peer support program, and are developing an app called “Enso” to offer real-time assessment and stress relief strategies, direct access to counselors for individual and family support through the Faculty and Employee Assistance Program (FEAP), and of a sort of “stress GPS” so units where adversity is high get the direction and help they need.
-54%
Reduction in STICU staff turnover after Wisdom & Wellbeing principles were rolled out in 2019
Wisdom and Wellbeing’s power comes in both granular and universal ways. Identifying a hospital unit’s most apparent stressors—unnecessary electronic documentation, for example, understaffing, or consistently unrealistic goals and expectations—enables practice changes, improves cohesion, and invests in team members’ wellness and longevity. Turnover due to stress, Westphal estimated, costs about $220,000 per nove nurse per year, but because these peer support programs stem attrition, they actually save money. In 2019, the results of a pilot pper support program using the Wisdom and Wellbeing principles reduced its annual turnover by more than 50%.
“Fundamentally,” said Plews-Ogan at a Medical Center Hour lecture last November, “people are not expendable. They are worthy of the attention required to help them be their best.”
Physical innovations, too, are popping up, and when space limitations or construction inhibit them, nurses like Muir, Nancy Farish, and Jeanell Webb-Jones build novel work-arounds. Early next month, new “Mobile Resiliency Toolboxes”—packed with virtual reality headsets and recordings of nature sounds, among other things—will offer another path for clinicians to take a break. Developed with clinicians’ input, the trio will deploy the boxes across three selected units by asking nurse managers to champion their use during shift huddles. With support from Chief Nursing Officer Mary Dixon, the trio will study the boxes’ uptake and impact.
+51%
The increase in applications to UVA's BSN program since last year
A Destination Still
Despite and perhaps because of the pandemic, nursing’s magnetism still beckons, and programs across the globe are seeing application surges. At UVA, BSN applications increased by 51%, CNL, MSN, and post-MSN applicants increased by 46%, and there were significant gains in applicants seeking and committing to early admission at the School. Though about 80% of courses remain online this spring, in-person labs and clinical rotations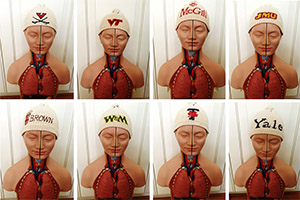 continue as nursing faculty continue to provide emotional support to students and create new ways to make Zoom personal, ceremonial, and fun.
continue as nursing faculty continue to provide emotional support to students and create new ways to make Zoom personal, ceremonial, and fun.
Last fall, professor Christine Connelly mailed secret envelopes with nursing assessment kits to all 81 first-years in her anatomy class. Over three sections on Zoom, Connelly had each student individually open and present their envelopes to reveal which “Hans” (that’s what Connelly calls the plastic anatomy mannequin) they’d received, which reflected what two- to three-member lab team they’d be part of, making ceremony of the groupings and offering an ice-breaker for new students, too.
“It really isn’t an understatement to say that nurses are literally saving the world,” said Beth Epstein (BSN `94, PhD `07), associate professor and interim director of academic programs. “It makes me feel really proud to be a faculty member teaching the future."
The Resilience Factor
Of course, no single solution will heal all that nurses have endured. There’s evidence, though, that taking time for mindfulness practices exerts a scientifically verifiable difference. Some of that research is being done at UVA.
Post-doctoral research associate Ebru Cayir and her Compassionate Care Initiative colleagues found in a study last June that clinicians exposed to stress who practiced The Pause—a mindfulness practice pioneered by UVA nurse Jonathan Bartels—toggled more readily between their brains’ sympathetic (“fight or flight”) and parasympathetic (“rest and digest”) nervous systems, implying an improved ability to cope with stress. The research group is getting ready to disseminate its findings soon.
“If we remain under stress for a long time without being able to effectively cope with it, our bodies become hypervigilant, and we can’t make balanced decisions,” explained Cayir. “That explains burnout, PTSD, mental health problems, mental illness. The more you think you can’t take a break, even 30 or 45 seconds, the more you probably need it.”
The work provides additional affirmation to those who say the resilience lessons they learned during nursing school stuck—and helped.
 “I remember when we went to UVA’s Morven Farms and . . . just had a self-care day with our clinical groups,” said Alderfer. “I’ve remembered that multiple times lately as I try to prioritize self-care these days. They’re really simple things: move, eat good food, spend time with people. Having had that tangible space and experiences in a beautiful place have really helped me prioritize. Actually having that experience that day has helped me.”
“I remember when we went to UVA’s Morven Farms and . . . just had a self-care day with our clinical groups,” said Alderfer. “I’ve remembered that multiple times lately as I try to prioritize self-care these days. They’re really simple things: move, eat good food, spend time with people. Having had that tangible space and experiences in a beautiful place have really helped me prioritize. Actually having that experience that day has helped me.”
“I do think I’ve taken UVA’s lessons with me,” said Meredith Bond (BSN `20), a pediatric ICU nurse in Atlanta, “by trying not to take too much of work home, and taking time for self-care, and just being able to have quiet moments by myself after a long day or night of work.”
Talia Sion (BSN `18), though aged by the COVID spring of 2020, feels a similar crackle of wisdom.
“We’ll live with this forever,” said Sion, now a labor and delivery nurse in New Jersey. “My first year as a nurse after graduation, there were times I wanted to quit, and throw in the towel—so normal for a new nurse. That 'new grad anxiety' came back in full force this past spring, as I found myself working during a global pandemic—but then I remembered that the work we do is epic in the literal sense of the word. What we do is important.”
Sion helps laboring women just one floor above where she worked last spring and summer on an all-COVID unit. She often takes the elevator down to see former colleagues, now her best friends. They hug. They talk. Sometimes they cry. And then they peel off their gowns and gloves and masks when they leave one another, steady themselves, and keep going.
“You go through hardship, but the things that brought you joy still bring you joy,” Sion insisted. “Sometimes I look back and think, ‘How did I survive?’ I don’t know. But guess what? I did.”







