
A Screening to Dismantle 'Involuntary Noncompliance'
Qaashuntae Wright (DNP `23) calls it “involuntary noncompliance”: when a patient doesn’t show up. Take their meds. Heed healthcare advice.
80%
of variations in health outcomes are attributed to social determinants of health (1)
Not because they don’t want to, but because they can’t. Nurses, she said, see it all the time.
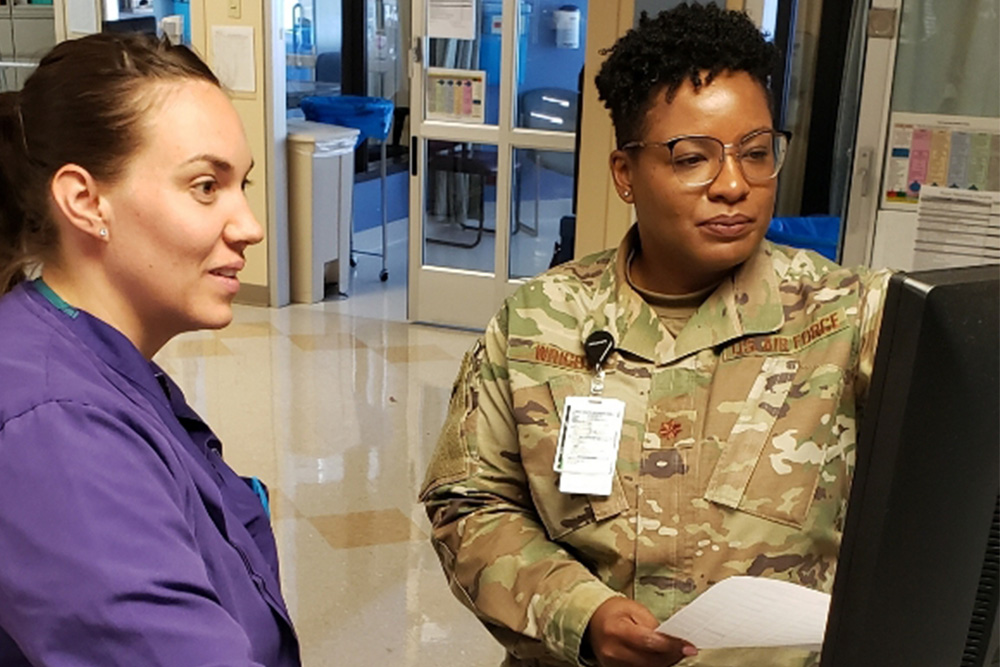
“It haunts me,” said Wright, an Air Force Major and nurse practitioner who goes by the nickname “Q.” “Being a nurse, you understand people don’t always have the necessary things they need to get the proper care, but as an ICU nurse, I want to know how my patients got there, to go back to their beginnings.”
Her hunch? Unmet social needs.
Two in three Americans will experience at least one unmet social need during their lives. [2] Maybe we can’t pay our rent or utilities, have a car that breaks down, lose a job, or experience violence. These pressing social and economic issues impact our health and are linked to higher expenditures for conditions like cardiovascular disease, kidney disease, and diabetes, an increased risk for hospitalization, and ER overuse. Unmet social needs make it harder to manage runaway chronic conditions, making it more likely we’ll die prematurely. [3]
While social services agencies—food banks, mental health clinics, government agencies that offer shelter and financial support—are well-positioned to help, many patients still fall through the cracks. One reason is that clinicians don’t often screen them, Wright said, despite increasing awareness of the impact that these factors exert on people’s wellbeing. Most healthcare workflows don’t make room for such screenings: only one-quarter of U.S. hospitals and 16% of private practices report screening patients for social needs [4], even though nearly nine in 10 healthcare providers believe addressing social needs is important. [5] Wright calls that a missed opportunity.
Only 25% of U.S. hospitals and 16% of private practices
report screening patients for social needs (4)
“The screening is a simple and streamlined way to open the door to conversations to meet standards and get things done,” she said, “to ask the patients, ‘Hey, do you have what you need?’ and go from there.”
While social needs screenings are considered best practice, exactly how they should be done is left up to individual clinicians, which clouds results. Questions might be too specific (“Do you have a car?”), too vague (“Any problems at home?”), or ill-fitting to the person. They can be difficult to integrate into electronic health records (EHR). They can even be off-putting to patients, make them clam up, get angry, or tune out—all reasons that Wright, on clinical rotation at a UVA dialysis clinic, wanted to try something new.
Wright deployed a “Core 5” social needs screening at the clinic, a two-minute protocol created by the Ohio Action Coalition and Robert Wood Johnson Foundation’s Public Health Nurse Leaders program. She trained clinic staff on its administration and aims. The nurse-delivered questions were simple, standardized, but heavy-hitting: focusing on transportation, food, housing, utilities, and safety.
Wright also tailored the tool for the dialysis clinic. In addition to adjusting questions’ cadence (asking more frequently about transportation problems, for example, which occur more frequently in patients receiving dialysis), she also standardized the words. So, “Do you have electricity?” became, “Are you currently having any concerns at home with your utilities, such as heat, electricity, natural gas, or water?” Completed on paper, unmet needs were input into the EHR as nurses’ notes for social worker to follow up on.
Wright screened 73 patients using the tool. Over the six-week study, she identified more than twice as many unmet social needs—a 120% increase—as the clinic’s previous tool, and dramatic increases in the number of patients connected with resources. Clinic nurses said it fit well into their workflow, and social workers liked it, too. Energized by Wright’s screening success, clinic leaders plan to deploy the tool across all 12 UVA dialysis clinics this summer, and Wright’s article about the work was accepted for publication in the Journal of Nursing Care Quality.
The project “motivated us to move forward to use some more clinically validated ways to ask questions, making us look at social determinants of health, which medical communities are saying is important,” said Michelle Monk, a clinic social worker. “Nothing is stagnant; things change, people’s needs change, so if there are improvements we can make, we definitely want to.”
The project “motivated us to move forward to use some more clinically validated ways to ask questions, making us look at social determinants of health, which medical communities are saying is important. Nothing is stagnant; things change, people’s needs change, so if there are improvements we can make, we definitely want to.”
Michelle Monk, a UVA Health dialysis clinic social worker
“Even when we told Q that we had a screening tool, she kept saying, ‘You’re not looking deep enough, we have to look at this more in depth,’” said Kim Deaver, who oversees all 12 of UVA Health’s dialysis clinics, which see more than 850 patients a year. “We were like, ‘OK, you show us.’ And she did. She went to the nth degree to show us: research is important.”
The promise is great. When social needs are met, patients’ conditions improve, and they may be able to stop symptom progression or even turn their conditions around. Nearly two in three of those Wright more effectively screened for social needs were the sometimes hard-to-reach population of older, Black men—men who could easily have been Wright’s stepfather, who died at 49, or her grandfather, who died in his early 50s, a fact that struck home.
“[My family members] would still be around if they’d had this kind of care,” Wright said. “This is what my career as a nurse is about.”

SOURCES
[1] Iott, B. E., Eddy, C., Casanova, C., & Veinot, T. C. (2021). More than a database: Understanding community resource referrals within a socio-technical systems framework. American Medical Informatics Association’s annual symposium proceedings. 583-592. https://pubmed-ncbi-nlm-nih-gov.proxy1.library.virginia.edu/33936432/
Jacobs, Z. G. (2021). Codifying social determinants of health: A gap in the ICD-10-CM. Journal of General Internal Medicine, 36(10), 3205-3207. doi:10.1007/s11606-021-06742-4
McGinnis, J. M., Williams-Russo, P., & Knickman, J. R. (2002). The case for more active policy attention to health promotion. Health Affairs, 21(2), 78-93. doi.org/10.1377/hlthaff.21.2.78
[2] MacDonald, I. (June 7, 2019). Rise Health. Social determinants of health: 68% of Americans surveyed have experienced at least one unmet social need in the past year. Retrieved from https://www.risehealth.org/insights-articles/social-determinants-of-health-68-of-americans-surveyed-have-experienced-at-least-one-unmet-social-need-in-the-past-year/
[3] Artiga, A., & Hinton, E. (May 10, 2018). Kaiser Family Foundation News. Beyond health care: The role of social determinants in promoting health and health equity. Retrieved from https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/
[4] Sufrin, C., Davidson, A., & Markenson, G. (January 2018). American College of Obstetricians and Gynecologists. Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. Retrieved from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/01/importance-of-social-determinants-of-health-and-cultural-awareness-in-the-delivery-of-reproductive-health-care
[5] Leventhal, R. (June 23, 2020). Healthcare Innovation. At reading hospital, addressing SDOH becomes a top priority. Retrieved from https://www.hcinnovationgroup.com/population-health-management/social-determinants-of-health/article/21143318/at-reading-hospital-addressing-sdoh-becomes-a-top-priority
